Udsa Beef Consumption by Year 1987
Meat intake varies widely throughout the world. In the USA and other developed countries, meat comprises a significant portion of the normal diet, contributing more than 15 % to daily energy intake, 40 % to daily protein intake and 20 % to daily fat intake( 1 – 3 ). The demand for meat in developing countries continues to grow as the production and consumption of meat increases with available income( Reference Walker, Rhubart-Berg and McKenzie 4 , Reference Speedy 5 ). A shift towards a dietary pattern characterized by high meat consumption also appears to supplant the consumption of cereals and other foods of plant origin( 1 , Reference Krebs-Smith 6 , Reference Terry, Terry and Wolk 7 ).
Early ecological comparisons provided the first indication that high meat consumption correlated with higher rates of chronic disease( Reference Dwyer and Hetzel 8 , Reference Armstrong and Doll 9 ), including CVD and cancer, the current leading causes of morbidity and mortality in the USA and other Westernised countries( 10 ). Health risks associated with meat consumption vary based on the animal the meat is derived from, as well as rearing, processing and preparation methods( Reference Bender 11 ). Meat can be further classified by the quantity of red v. white muscle fibres; thus, beef, pork and lamb products are generally defined as red meat and poultry products as white meat. Preparation methods such as smoking, curing, salting and/or addition of preservatives further differentiate processed and fresh meat( Reference Bender 11 ). The components of meat linked to chronic disease risk include fat content, particularly saturated fat in red meat, and dietary cholesterol( Reference Hu, Stampfer and Manson 12 , Reference Lichtenstein, Appel and Brands 13 ). Meat can also be a source of several known mutagens, including N-nitroso compounds (NOC) in processed meats, and heterocyclic amines (HCA) and polycyclic aromatic hydrocarbons (PAH) formed during high-temperature cooking and grilling( Reference Cross and Sinha 14 ).
Intake of fat and meat (primarily from red meat) has been of public health concern since the late 1950s when the American Heart Association first recommended that dietary cholesterol, saturated fat and total fat be reduced for the prevention of CVD( Reference Lichtenstein, Appel and Brands 13 , 15 ); and to date, numerous epidemiological studies have investigated meat intake and cancer risk( Reference Alaejos, Gonzalez and Afonso 16 – Reference Larsson and Wolk 19 ). According to the World Cancer Research Fund/American Institute for Cancer Research report in 2007, the evidence linking red and processed meats to colorectal cancer was deemed 'convincing' and 'limited or suggestive' for other cancer sites( 20 ).
Based on the evidence to date, current dietary recommendations for the prevention of diet-related chronic diseases( 20 – Reference Reedy and Krebs-Smith 23 ) suggest to limit intake of red and processed meat and to eat mostly foods of plant origin. The present study describes the trends, distribution and potential determinants of meat consumption within the USA and other parts of the developed world over the past several decades. Further discussion addresses recent epidemiological evidence for meat intake and chronic disease risk, and impending public health concerns.
Methods
We used publicly accessible per capita food availability data provided by the FAO( 24 ) and the US Department of Agriculture (USDA)( 25 ) to compare temporal trends in meat consumption in the USA and other developed countries (defined by the FAO as Japan in Asia, Canada and the USA in North America, Australia and New Zealand in Oceania, and all of Europe). FAO and USDA databases provide historical and chronological population-based production and disappearance data (referred to as food availability or consumption). We compared temporal trends in the US meat disappearance data to dietary intake data collected at the individual level from the National Health and Nutrition Examination Surveys (NHANES)( 26 ).
FAO
FAOSTAT( 24 ) is the world's largest online agricultural database (available at http://faostat.fao.org/) with data from 190 FAO member countries. FAO compiles supply and disappearance data submitted by member countries in response to standard questionnaires, supplemented with reviews of national sources and staff estimates or imputations to cover critical gaps( Reference Speedy 5 ). The FAO classifies total meat (excluding fish) as the sum of beef, poultry, pork, sheep, goat and other game. Per capita meat consumption (g/d), defined as the total amount of the commodity available for human consumption (i.e. after exports, and other waste from farm to household), was available from 1961 through 2005. Data from 1990 were revisited, resulting in changes in the historical data. The methodology for the estimation of food balance sheets was also revised in FAOSTAT, including new aggregation techniques for the conversion of transformed commodities (processed and semi-processed) into primary equivalents (i.e. fresh meat, excluding offal and fat)( 24 ).
US Department of Agriculture
To look at US meat consumption and trends in more detail, we referenced food availability data (also known as US Food Supply Data or Disappearance Data) from the USDA Economic Research Service (ERS) and accessible at http://www.ers.usda.gov/Data/Foodconsumption ( 25 ). The ERS food data system reflects food availability per capita on an annual basis from 1909 through 2007 at the national level and serves as a popular proxy for actual consumption. These data represent the boneless, trimmed (edible) weight of fresh meat. Loss-adjusted data (removal of non-edible food parts and food lost through spoilage, plate waste and other losses in the home and marketing system) were only available beginning from 1970. Red meat commodities included beef, veal, pork, lamb and mutton. Poultry commodities included turkey and chicken. Fish and shellfish included fresh and frozen, canned and cured products. Figures were calculated on the basis of raw and edible meats, which exclude edible offal, bones and viscera for red meat and fishery products, but included skin, neck and giblets for poultry( 25 ). The USDA per capita data, provided in lb/year, were converted to g/d (453·6 g/lb; 365·2 d/year) for the sake of comparison with other data sources.
National Health and Nutrition Examination Surveys
We examined data from NHANES for 1999–2000 (8074 people), 2001–2002 (9033 people) and 2003–2004 (8273 people). NHANES is a cross-sectional national survey conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. The dietary portion was designed to provide nationally representative estimates of food intake in adults and children (civilian, non-institutionalized population), and to track changes in health and nutritional status over time. A single 24 h dietary recall from all respondents aged 2 years and older with reliable dietary data was included and appropriate weighting factors were applied to adjust for differential probabilities of selection and non-response. Additional information on the survey designs, data collection protocols, weighting procedures and response rates is given elsewhere( 26 ).
To estimate meat intake we merged the NHANES data with the appropriate MyPyramid Equivalents Database (MPED). A new version of the MPED is developed for each NHANES data release; thus, MPED 1·0( Reference Friday and Bowman 27 ) was applied to survey data before 2002 and MPED 2·0( Reference Bowman, Friday and Mosehfegh 28 ), the most current version available, to 2003–2004. MPED for USDA Survey Foods translates the amounts of foods eaten in USDA's What We Eat in America survey, the dietary intake component of NHANES, into the number of equivalents for the thirty-two MyPyramid major food groups and subgroups( Reference Bowman, Friday and Mosehfegh 28 ). Meat intake reported in the 24 h dietary recall is converted to the equivalent number of cup or ounce equivalents (servings) after disaggregating mixtures and discretionary fats. Allowable fat in the meat group includes that present in lean cuts of meat trimmed of all fat and poultry without skin. Cooked lean meat ounce equivalents (servings) were defined as no more than 9·28 g fat per 100 g of meat, poultry or fish, or 3·53 ounces of cooked lean meat per 100 g of product, with the remainder classified as discretionary fat( Reference Bowman, Friday and Mosehfegh 28 ). MPED estimates were converted to g/d (28 g/oz). We used the following food group variables from the database: meat, poultry, fish with high n-3 fatty acid content, fish with low n-3 fatty acid content and processed meat. The poultry group consisted mainly of chicken and turkey. Total fish was the sum of fish both high and low in n-3 fatty acids plus shellfish. To generate a total red meat variable, we included red meat (beef, pork, veal, lamb, game), as well as the appropriate components of processed meat and organ meats, based on the recipe files for each of the food items in these food categories. Similarly, a total white meat variable was generated from poultry and processed or organ components from each of these groups. Total meat was the sum of fresh (not processed) red and white meat, plus cured meat, such as bacon and ham, as well as organ meats and fish. Soya products were excluded. Processed meat, by MPED definition( Reference Bowman, Friday and Mosehfegh 28 ), included frankfurters, sausage and luncheon meats (made from meat or poultry), but did not include cured meats, such as ham or bacon.
We used SUDAAN (Research Triangle Institute (RTI) International, Research Triangle Park, NC, USA) to generate weighted means (sampling weights provided by NHANES)( 26 ) and standard errors for each meat item (red meat, poultry, fish and processed meat; g/d). We additionally examined meat intake stratified by gender, age group, ethnicity and education level. Using a Bonferroni correction to adjust for multiple comparisons, a two-sided P < 0·0005 was considered statistically significant for any single pair-wise comparison.
Results
Temporal trends in meat consumption in developed countries
According to the international FAO data, total meat consumption (excluding fish) in the USA, European Union (EU) and the developed world as a whole has increased relatively steadily over the period from 1961 to 2003 (Fig. 1). As early as 1961, total meat consumption in the USA was nearly double that of the EU and the developed world as a whole. From 1961 to 2003, total meat consumption continued to increase in all regions: nearly doubling in the EU and increasing approximately 1·5-fold in the USA. Overall, meat consumption appears to be on the rise in the developed world as whole, but remains considerably lower than in the USA.

Fig. 1 Total meat consumption in the USA, European Union and the developed world, 1961–2003 (FAOSTAT( 24 ))
Looking in more detail at meat consumption in the USA, USDA data indicate that total meat consumption has increased notably over the past century, nearly doubling between 1909 and 2007 (Fig. 2). The lowest meat consumption occurred in the 1930s and the highest meat consumption was reached during the most recent decade. Further examination attributes much of the increase to a rise in poultry consumption beginning in the 1950s through recent decades to make up a high proportion of the total meat consumed in the USA. Red meat consumption appears to have decreased over the past few decades beginning in the 1980s, but still remains the highest contributor to the total meat consumed. In contrast, fish consumption has remained low and stable over the past century.
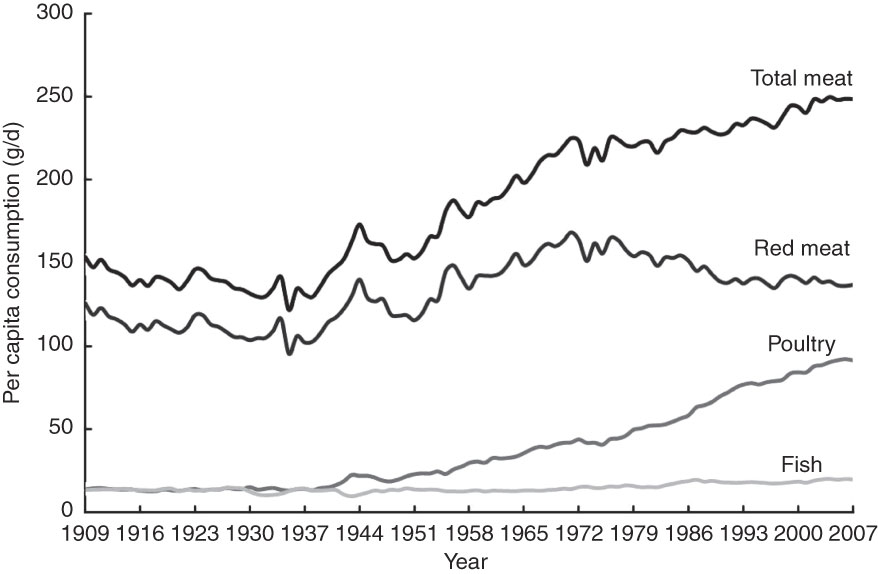
Fig. 2 Total meat, red meat, poultry and fish consumption in the USA, 1909–2007 (US Department of Agriculture, Economic Research Service( 25 ))
The same data adjusted for loss, but only available from 1970, are comparable to the trends shown in Fig. 2 with a marked increase in poultry consumption, a slight decrease in red meat consumption and an overall trend for increasing meat consumption. For the period 1970–2007, per capita red meat consumption dropped from 105 to 85 g/d, while per capita poultry consumption more than doubled from 25 to 55 g/d (loss-adjusted data not shown). Per capita total loss-adjusted meat consumption was highest in 2004 at 154 g/d with current estimates remaining close to this value (data not shown).
Components and determinants of meat consumption in the USA
The NHANES (2003–2004) data from a single 24 h dietary recall indicate that approximately 58 % of the meat consumed in the USA was red meat, 32 % poultry and 10 % fish (Fig. 3). Processed meat intake constituted 22 % of the total meat consumed from either red meat or poultry categories. Women consumed a slightly higher proportion of poultry than men (34 % and 30 %, respectively), a lower proportion of red meat (55 % and 60 %, respectively) and nearly equal proportions of processed meat (data not shown).

Fig. 3 Percentage intake of different types of meat in the USA estimated by a single 24 h dietary recall, National Health and Nutrition Examination Survey, 2003–2004: (a) distribution of meat types that contribute to total meat intake; (b) percentage of total meat that is processed
Table 1 describes US meat intake from NHANES (2003–2004) by gender, age, ethnicity and education level. In this nationally representative sample, total meat intake averaged 128 g/d (sum of red meat, poultry and fish). Compared with women, men consumed more of every type of meat per day (all pair-wise comparisons (not shown) were statistically significant (P < 0·0005)). With the exception of fish, peak meat consumption occurred in adults aged 20–49 years, particularly for red meat (80·3 g/d), with lower intake at younger and older ages (P < 0·0005 for ages 20–49 years compared to ≥70 years for red meat, poultry, total meat and processed meat). Whites, Blacks and Hispanics all reported similar intake of red meat. Blacks consumed the highest amount of poultry (54·4 g/d) compared to Whites (P < 0·0005) and Hispanics (P < 0·001, NS for multiple comparisons). Hispanics reported lower processed meat intake than Whites (P < 0·001 (NS)) and Blacks (P < 0·0005). Poultry and fish consumption appeared to increase with education level. Results between 1999–2000 and 2001–2002 were not notably different from the 2003–2004 results presented here. Across the 1999–2000, 2001–2002 and 2003–2004 surveys, red meat intake appeared to decrease slightly, while poultry intake appeared to increase slightly (data not shown), which is in agreement with the data from the USDA (Fig. 2).
Table 1 Meat intake in the USA according to demographic factors, National Health and Nutrition Examination Survey, 2003–2004

*Cooked lean meat ounce-equivalents (MPED 2·0) converted to grams.
Discussion
Food availability data indicate that overall meat consumption is on the rise in the developed nations of the world and that the USA remains the highest consumer of total meat. Despite a shift towards increased poultry consumption, red meat still represents the largest proportion of meat consumed in the USA and nearly a quarter of the meat consumed is processed. Meat selection and consumption behaviours appeared to vary by education, race, age and gender.
Despite the near record-high per capita consumption of total meat in recent years, the proportion of fat, particularly saturated fat, in the US food supply from meat, poultry and fish has slowly declined( 3 ). Public health and consumer concerns regarding fat and cholesterol in the late 1980s led to greater demand for lean meat and poultry, increased trimming of visible fat on meat at the retail level and consumer substitution of poultry for red meat( 3 , 29 ). Reports on fat consumption trends in the USA have shown a marked reduction in the proportion of fat from foods identified as major sources of saturated fat, including red meat (pork and beef) over the past several decades( Reference Popkin, Siega-Riz and Haines 30 , Reference Chanmugam, Guthrie and Cecilio 31 ).
Previous reports have shown that the consumer's knowledge and awareness of diet and health may affect the proportion of red v. white meat consumed both at home and away from home( Reference Lin, Yen and Davis 32 ). Chronological USDA data suggest that although poultry consumption has increased, red meat consumption has decreased comparably little, leaving total meat consumption on the rise. Both loss-adjusted USDA data and intake values in NHANES suggest that current total meat intake for adults in the USA ranges from 100 to 150 g/d with more than half (50–90 g/d) coming from red meat. The affordability of meat in the USA, combined with rising consumer incomes, may explain this trend. While vertical integration in US poultry production resulted in a large, low-cost supply of poultry, the USA remains the world's largest beef producer and exporter, as well as a leading beef importer( 3 , Reference Brester, Marsh and Plain 33 ). During 1994–1996, beef was a close second to yeast bread as the leading source of energy in US adults; and the primary source of both protein and total fat( Reference Cotton, Subar and Friday 34 ). Meat consumption, production and trade flows are also subject to temporary fluctuations due to food safety issues. The outbreak of bovine spongiform encephalopathy or 'mad cow disease' identified in the UK in the 1980s and later in the USA (2003) was a considerable blow to the beef industry and trade( Reference Nathanson, Wilesmith and Griot 35 , Reference Harman and Silva 36 ).
The NHANES data suggest that recent patterns of meat intake and overall consumption differ within the US population according to various demographic factors, reflecting perhaps cultural, social, regional and financial influences on diet. NHANES may provide a different picture of meat intake in US individuals than have large, US prospective cohorts, whose participants are largely Caucasian, age 50 years or above, and college educated. Although at a national level the demand for meat would be expected to increase with economic growth, individual intake has tended to level off, and may even decline, at the highest levels of socio-economic status( Reference Purcell and Lusk 37 ). Lower meat intake, particularly red and processed meat, with increasing adult age and education may reflect heightened awareness of health and/or adoption of dietary practices for the prevention or management of chronic disease.
Possible health implications of meat consumption
Meat in the diet provides an important source of protein and micronutrients, such as iron, zinc and vitamin B( Reference Stipanuk 38 ). However, energy-dense diets, purported to be high in meat, fats and sugars, and further compounded by sedentary lifestyle, have been implicated in the growing epidemics of obesity and diet-related chronic diseases( 20 , Reference Mente, de Koning and Shannon 39 ). Evidence suggests that vegetarians may be at lower risk for CVD, hypertension, diabetes mellitus, obesity and some cancers( Reference Fraser 40 – Reference Key, Appleby and Spencer 44 ). However, low-fat/high-carbohydrate diets have not been wholly positive or successful in reducing the burden of chronic disease within the general population( Reference Hodgson, Burke and Beilin 45 – Reference Siri-Tarino, Sun and Hu 47 ); and lean meat and fish continue to be part of the recommendations for a balanced, healthy diet( Reference Lichtenstein, Appel and Brands 13 , Reference Kant and Graubard 48 ).
Inflammation and oxidative stress have also been linked to the intake of meat and disease risk. Red meat, possibly due to its fat and iron content, may increase inflammation and oxidative stress, but less is known regarding lean and white meats( Reference Szeto, Kwok and Benzie 41 , Reference Hodgson, Ward and Burke 49 ). Conversely, the intake of fish has been shown to decrease markers of inflammation and oxidative stress( Reference Lopez-Garcia, Schulze and Manson 50 , Reference Wijendran and Hayes 51 ). Meat cooking (high temperature, charring) and processing techniques, such as smoking, curing, salting or the addition of chemical preservatives, lead to the formation of carcinogenic compounds, such as NOC, HCA and PAH( Reference Cross, Leitzmann and Gail 17 , Reference Stolzenberg-Solomon, Cross and Silverman 52 , Reference Sinha and Norat 53 ). Exposure to NOC occurs from both endogenous formation, which is directly related to red meat intake( Reference Hughes, Cross and Pollock 54 ), as well as exogenous exposure from nitrite-preserved meats( Reference Mirvish, Haorah and Zhou 55 ). Nitrate, which can be reduced to nitrite and contribute to NOC formation, is also present in non-meat sources, such as vegetables and fruits( Reference Hord, Tang and Bryan 56 ); however, red meat is a key source of readily available haem iron, which may further increase endogenous NOC formation( Reference Cross, Pollock and Bingham 57 ). HCA and PAH, which are formed during high-temperature cooking of meat( Reference Sinha, Rothman and Salmon 58 ), dose-dependently generate DNA adducts( Reference Turteltaub, Dingley and Curtis 59 ).
The most robust human evidence is for red and processed meat intake and colorectal cancer( Reference Larsson and Wolk 19 , 20 , Reference Norat, Bingham and Ferrari 60 – Reference Larsson, Rafter and Holmberg 64 ). To date, there appears to be little or no association for meat intake and breast cancer( Reference Linos and Willett 65 – Reference Pala, Krogh and Berrino 69 ), while findings for other major cancers such as prostate, lung, kidney and pancreatic cancer are less conclusive( Reference Lee, Spiegelman and Hunter 70 – Reference Sinha, Park and Graubard 73 ). In a comprehensive investigation from a US prospective study of over 500 000 men and women, a significant increased risk of incident cancers of the colorectum, oesophagus, lung and liver was associated with red meat and increased risk of colorectal and lung cancer was associated with higher intake of processed meat( Reference Cross, Leitzmann and Gail 17 ); red and processed meat intake was also associated with all-cause, CVD and cancer mortality, while higher intake of white meat was associated with lower risk of death( Reference Sinha, Cross and Graubard 74 ). The relationship between meat intake and cancer risk is not wholly consistent and the complex mechanisms involved continue to warrant further investigation. Current epidemiological research suggests that moderate meat intake may not increase risk( Reference Spencer, Key and Appleby 75 ) and that endogenous and exogenous mutagens formed during meat cooking and processing may be important( Reference Sinha and Norat 53 , Reference Cross, Ferrucci and Risch 61 , Reference Pala, Krogh and Berrino 69 , Reference Sinha, Park and Graubard 73 , Reference Truswell 76 , Reference Genkinger and Koushik 77 ).
Strengths and limitations
Results presented herein should be viewed with caution and the limitations of food supply/disappearance and cross-sectional data clearly acknowledged. There are a number of disadvantages to using food availability data, even though it is important for international comparisons as well as for looking at the overall, historic trends. Meat consumption data presented here are primarily based on annual food availability per capita at the national level and serve as popular proxies for actual consumption. The FAO derives their values from data submitted by member countries and are therefore limited by the completeness and accuracy of reporting at the national level.
It is important to recognise that while each data source appears to tell a similar story of US meat consumption trends, USDA food availability and NHANES individual intake data serve different objectives( Reference Popkin, Siega-Riz and Haines 30 ). The US food availability and consumption data measure the flow of raw and semi-processed agricultural commodities throughout the US marketing system at an aggregate level( Reference Kantor 78 ). For both FAO and USDA food consumption data, human food intake is not directly measured and losses from trimming, cooking, waste and spoilage are not fully estimable despite use of conversion factors that attempt to adjust for probable losses; this appeared to result in as much as a 100 g difference between current adjusted (150 g/d) and unadjusted USDA values (250 g/d). Individual-level intake data, such as those collected in NHANES from individual sample respondents, measure only edible and reportedly consumed foods from a designated period or point in time. In a large sample, such as NHANES, a single 24 h dietary recall should provide a valid estimate of total meat intake at a population level and should also be adequate to capture relative consumption of different types of meat( Reference Sekula, Nelson and Figurska 79 , Reference Basiotis, Welsh and Cronin 80 ). The NHANES population itself presents a number of advantages for studying current US meat intake. The NHANES sampling aims to capture the diversity, as well as regional variation in the US population. Younger age groups and minority populations sampled in NHANES are often under-represented in most large epidemiological and US prospective studies. In addition, most prospective cohorts in the USA and Europe began in the mid 1980s to 1990s, serving as the baseline level of intake, which USDA and NHANES data suggest may be considerably lower than the current US intake. Thus, comparably modest associations with meat in cohort populations may or may not translate to the broader US population, which national estimates suggest may be at differential, if not greater, risk in the near future.
Although historical food availability data may not be a precise representation of intake, the measurement methodology has remained relatively consistent over time. Thus, comparing FAO and USDA data with NHANES data is a useful way to corroborate changing meat consumption patterns and trends( Reference Chanmugam, Guthrie and Cecilio 31 ). For the period 2003–2004, we found similar meat intake patterns for the relative proportion of types of meat consumed from both USDA and NHANES data. Unfortunately, the lag in the development and linkage of the MPED, the USDA's food group database, limits our ability to present NHANES meat intake data beyond 2003–2004. NHANES was the only data source in our analysis that shed light on processed meat intake and although it appears to make up a high proportion of the total meat currently consumed, we are unable to track long-term changes in its availability and consumption. USDA and FAO tracking methods, by nature, do not allow for historical trend data on meat that has undergone processing, which may be derived from both fresh red meat and poultry. Due to emerging epidemiological evidence on the risks of various cancers associated with high processed meat intake, recommendations to reduce consumption of processed meat are relatively new compared to those for red meat. In addition, there is no generally agreed upon definition of processed meat, making it difficult to define and target in both public health research and practice.
Conclusion
Understanding the trends and determinants of meat consumption in the USA, where meat is consumed at more than three times the global average( Reference Speedy 5 ), should be particularly pertinent to researchers and other public health professionals aiming to reduce the global burden of chronic disease. While saturated fat intake appears to be declining( 3 , 29 – Reference Chanmugam, Guthrie and Cecilio 31 ), other components of red and processed meat continue to pose a health risk, particularly when consumed in large quantities( Reference Cross, Leitzmann and Gail 17 , Reference Stolzenberg-Solomon, Cross and Silverman 52 – Reference Mirvish, Haorah and Zhou 55 , Reference Cross, Pollock and Bingham 57 – Reference Turteltaub, Dingley and Curtis 59 ). Dietary recommendations for meat should perhaps begin to increase awareness regarding potentially harmful cooking and processing methods( Reference Cross and Sinha 14 , Reference Sinha and Norat 53 ). Studying food consumption and selection behaviours sheds light on the barriers we continue to face with the food industry and consumers, as well as international foresight into future epidemics and their causes. As the main determinant of per capita meat consumption across the world appears to be wealth, examining trends in the USA and the rest of the developed world may forecast the global public health and environmental burdens we should expect to face in the highly populated developing world( Reference Walker, Rhubart-Berg and McKenzie 4 ). The growing preference in the USA for poultry, but not fish, as a replacement for red meat suggests the need for more epidemiological investigations of white meat and its relationship with long-term health and disease outcomes.
Acknowledgements
The present study was supported by the Intramural Research Program of the NIH, National Cancer Institute. None of the authors had a financial or personal conflict of interest. C.R.D. contributed to the concept, analysis, interpretation of results and writing of the manuscript; A.J.C. contributed to the interpretation of results and writing of the manuscript; C.K. helped the analysis and interpretation of the results; R.S. contributed to the concept, interpretation of the results and writing of the manuscript; and all authors contributed to the critical review and approval of the final manuscript. The authors thank Jill Reedy and Lisa Kahle for their contributions to this manuscript.
References
2. Hiza, HAB , Bente, L & Fungwe, T (2008) Nutrient content of the US food supply, 1909–2005. Home Econ Res Rep 58.Google Scholar
4. Walker, P , Rhubart-Berg, P , McKenzie, S et al. (2005) Public health implications of meat production and consumption. Public Health Nutr 8, 348–356.CrossRefGoogle ScholarPubMed
7. Terry, P , Terry, JB & Wolk, A (2001) Fruit and vegetable consumption in the prevention of cancer: an update. J Intern Med 250, 280–290.CrossRefGoogle ScholarPubMed
8. Dwyer, T & Hetzel, BS (1980) A comparison of trends of coronary heart disease mortality in Australia, USA and England and Wales with reference to three major risk factors – hypertension, cigarette smoking and diet. Int J Epidemiol 9, 65–71.CrossRefGoogle ScholarPubMed
9. Armstrong, B & Doll, R (1975) Environmental factors and cancer incidence and mortality in different countries, with special reference to dietary practices. Int J Cancer 15, 617–631.CrossRefGoogle ScholarPubMed
10. World Health Organization (2009) World Health Statistics. Geneva: WHO.Google Scholar
11. Bender, A (1992) Meat and Meat Products in Human Nutrition in Developing Countries. FAO Food and Nutrition Paper no. 53. Rome: FAO.Google Scholar
12. Hu, FB , Stampfer, MJ , Manson, JE et al. (1999) Dietary saturated fats and their food sources in relation to the risk of coronary heart disease in women. Am J Clin Nutr 70, 1001–1008.CrossRefGoogle ScholarPubMed
13. Lichtenstein, AH , Appel, LJ , Brands, M et al. (2006) Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 114, 82–96.CrossRefGoogle ScholarPubMed
14. Cross, AJ & Sinha, R (2004) Meat-related mutagens/carcinogens in the etiology of colorectal cancer. Environ Mol Mutagen 44, 44–55.CrossRefGoogle ScholarPubMed
15. American Heart Association (2008) American Heart Association Scientific Statements and Practice Guidelines for Researchers and Scientists: Diet/Nutrition. Dallas, TX: AHA Inc.; available at http://www.americanheart.orgGoogle Scholar
16. Alaejos, MS , Gonzalez, V & Afonso, AM (2008) Exposure to heterocyclic aromatic amines from the consumption of cooked red meat and its effect on human cancer risk: a review. Food Addit Contam Part A Chem Anal Control Expo Risk Assess 25, 2–24.CrossRefGoogle ScholarPubMed
17. Cross, AJ , Leitzmann, MF , Gail, MH et al. (2007) A prospective study of red and processed meat intake in relation to cancer risk. PLoS Med 4, e325.CrossRefGoogle ScholarPubMed
18. Huxley, RR , Ansary-Moghaddam, A , Clifton, P et al. (2009) The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer 125, 171–180.CrossRefGoogle ScholarPubMed
19. Larsson, SC & Wolk, A (2006) Meat consumption and risk of colorectal cancer: a meta-analysis of prospective studies. Int J Cancer 119, 2657–2664.CrossRefGoogle ScholarPubMed
20. World Cancer Research Fund/American Institute for Cancer Research (2007) Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective. Washington, DC: AICR.Google Scholar
21. Krauss, RM , Eckel, RH , Howard, B et al. (2001) Revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. J Nutr 131, 132–146.CrossRefGoogle ScholarPubMed
22. Kushi, LH , Byers, T , Doyle, C et al. (2006) American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 56, 254–281.CrossRefGoogle ScholarPubMed
23. Reedy, J & Krebs-Smith, SM (2008) A comparison of food-based recommendations and nutrient values of three food guides: USDA's MyPyramid, NHLBI's dietary approaches to stop hypertension eating plan, and Harvard's healthy eating pyramid. J Am Diet Assoc 108, 522–528.CrossRefGoogle ScholarPubMed
24. Food and Agriculture Organization of the United Nations (2008) FAO Statistical Databases (FAOSTAT). Food consumption data. http://faostat.fao.org/ (accessed December 2008).Google Scholar
28. Bowman, SA , Friday, JE & Mosehfegh, A (2008) MyPyramid Equivalents Database, 2.0 for USDA Survey Foods, 2003–2004. Food Surveys Research Group. Beltsville, MD: Beltsville Human Nutrition Research Center, ARS, USDA; available at http://www.ars.usda.gov/ba/fsrgGoogle Scholar
29. Committee on Technological Options to Improve the Nutritional Attributes of Animal Products, National Research Council (1988) Designing Foods: Animal Product Options in the Marketplace. Washington, DC: National Academy Press.Google Scholar
30. Popkin, BM , Siega-Riz, AM , Haines, PS et al. (2001) Where's the fat? Trends in US diets 1965–1996. Prev Med 32, 245–254.CrossRefGoogle Scholar
31. Chanmugam, P , Guthrie, JF , Cecilio, S et al. (2003) Did fat intake in the United States really decline between 1989–1991 and 1994–1996? J Am Diet Assoc 103, 867–872.CrossRefGoogle ScholarPubMed
32. Lin, BH , Yen, S & Davis, C (2006) Consumer Knowledge and Meat Consumption in the US. Gold Coast, Australia: International Association of Agricultural Economists.Google Scholar
33. Brester, GW , Marsh, JM & Plain, RL (2003) International red meat trade. Vet Clin North Am Food Anim Pract 19, 493–518.CrossRefGoogle ScholarPubMed
34. Cotton, PA , Subar, AF , Friday, JE et al. (2004) Dietary sources of nutrients among US adults, 1994 to 1996. J Am Diet Assoc 104, 921–930.CrossRefGoogle ScholarPubMed
35. Nathanson, N , Wilesmith, J & Griot, C (1997) Bovine spongiform encephalopathy (BSE): causes and consequences of a common source epidemic. Am J Epidemiol 145, 959–969.CrossRefGoogle ScholarPubMed
37. Purcell, WD & Lusk, J (2003) Demand for red meats: principles, research evidence, and issues. Vet Clin North Am Food Anim Pract 19, 463–492, viii.CrossRefGoogle ScholarPubMed
38. Stipanuk, M (1999) Biochemical, Physiological & Molecular Aspects of Human Nutrition, 2nd ed. Philadelphia, PA: W.B. Saunders.Google Scholar
39. Mente, A , de Koning, L , Shannon, HS et al. (2009) A Systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 169, 659–669.CrossRefGoogle ScholarPubMed
40. Fraser, GE (2009) Vegetarian diets: what do we know of their effects on common chronic diseases? Am J Clin Nutr 89, 1607S–1612.CrossRefGoogle ScholarPubMed
41. Szeto, YT , Kwok, TC & Benzie, IF (2004) Effects of a long-term vegetarian diet on biomarkers of antioxidant status and cardiovascular disease risk. Nutrition 20, 863–866.CrossRefGoogle ScholarPubMed
42. Key, TJ , Appleby, PN , Spencer, EA et al. (2009) Cancer incidence in British vegetarians. Br J Cancer 101, 192–197.CrossRefGoogle ScholarPubMed
43. Key, TJ , Appleby, PN , Spencer, EA et al. (2009) Mortality in British vegetarians: results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford). Am J Clin Nutr 89, 1613S–1619S.CrossRefGoogle Scholar
44. Key, TJ , Appleby, PN , Spencer, EA et al. (2009) Cancer incidence in vegetarians: results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford). Am J Clin Nutr 89, 1620S–1626S.CrossRefGoogle Scholar
45. Hodgson, JM , Burke, V , Beilin, LJ et al. (2006) Partial substitution of carbohydrate intake with protein intake from lean red meat lowers blood pressure in hypertensive persons. Am J Clin Nutr 83, 780–787.CrossRefGoogle ScholarPubMed
46. Appel, LJ , Sacks, FM , Carey, VJ et al. (2005) Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 294, 2455–2464.CrossRefGoogle ScholarPubMed
47. Siri-Tarino, PW , Sun, Q , Hu, FB et al. (2010) Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr 91, 535–546.CrossRefGoogle ScholarPubMed
48. Kant, AK & Graubard, BI (2005) A comparison of three dietary pattern indexes for predicting biomarkers of diet and disease. J Am Coll Nutr 24, 294–303.CrossRefGoogle ScholarPubMed
49. Hodgson, JM , Ward, NC , Burke, V et al. (2007) Increased lean red meat intake does not elevate markers of oxidative stress and inflammation in humans. J Nutr 137, 363–367.CrossRefGoogle Scholar
50. Lopez-Garcia, E , Schulze, MB , Manson, JE et al. (2004) Consumption of (n-3) fatty acids is related to plasma biomarkers of inflammation and endothelial activation in women. J Nutr 134, 1806–1811.CrossRefGoogle ScholarPubMed
51. Wijendran, V & Hayes, KC (2004) Dietary n-6 and n-3 fatty acid balance and cardiovascular health. Annu Rev Nutr 24, 597–615.CrossRefGoogle ScholarPubMed
52. Stolzenberg-Solomon, RZ , Cross, AJ , Silverman, DT et al. (2007) Meat and meat-mutagen intake and pancreatic cancer risk in the NIH–AARP cohort. Cancer Epidemiol Biomarkers Prev 16, 2664–2675.CrossRefGoogle ScholarPubMed
53. Sinha, R & Norat, T (2002) Meat cooking and cancer risk. IARC Sci Publ 156, 181–186.Google ScholarPubMed
54. Hughes, R , Cross, AJ , Pollock, JR et al. (2001) Dose-dependent effect of dietary meat on endogenous colonic N-nitrosation. Carcinogenesis 22, 199–202.CrossRefGoogle ScholarPubMed
55. Mirvish, SS , Haorah, J , Zhou, L et al. (2002) Total N-nitroso compounds and their precursors in hot dogs and in the gastrointestinal tract and feces of rats and mice: possible etiologic agents for colon cancer. J Nutr 132, 3526S–3529S.CrossRefGoogle ScholarPubMed
56. Hord, NG , Tang, Y & Bryan, NS (2009) Food sources of nitrates and nitrites: the physiologic context for potential health benefits. Am J Clin Nutr 90, 1–10.CrossRefGoogle ScholarPubMed
57. Cross, AJ , Pollock, JR & Bingham, SA (2003) Haem, not protein or inorganic iron, is responsible for endogenous intestinal N-nitrosation arising from red meat. Cancer Res 63, 2358–2360.Google ScholarPubMed
58. Sinha, R , Rothman, N , Salmon, CP et al. (1998) Heterocyclic amine content in beef cooked by different methods to varying degrees of doneness and gravy made from meat drippings. Food Chem Toxicol 36, 279–287.CrossRefGoogle ScholarPubMed
59. Turteltaub, KW , Dingley, KH , Curtis, KD et al. (1999) Macromolecular adduct formation and metabolism of heterocyclic amines in humans and rodents at low doses. Cancer Lett 143, 149–155.CrossRefGoogle ScholarPubMed
60. Norat, T , Bingham, S , Ferrari, P et al. (2005) Meat, fish, and colorectal cancer risk: the European Prospective Investigation into Cancer and Nutrition. J Natl Cancer Inst 97, 906–916.CrossRefGoogle ScholarPubMed
61. Cross, AJ , Ferrucci, LM , Risch, A et al. (2010) A large prospective study of meat consumption and colorectal cancer risk: an investigation of potential mechanisms underlying this association. Cancer Res 70, 2406–2414.CrossRefGoogle ScholarPubMed
62. Norat, T , Lukanova, A , Ferrari, P et al. (2002) Meat consumption and colorectal cancer risk: dose–response meta-analysis of epidemiological studies. Int J Cancer 98, 241–256.CrossRefGoogle ScholarPubMed
63. Chao, A , Thun, MJ , Connell, CJ et al. (2005) Meat consumption and risk of colorectal cancer. JAMA 293, 172–182.CrossRefGoogle ScholarPubMed
64. Larsson, SC , Rafter, J , Holmberg, L et al. (2005) Red meat consumption and risk of cancers of the proximal colon, distal colon and rectum: the Swedish Mammography Cohort. Int J Cancer 113, 829–834.CrossRefGoogle ScholarPubMed
65. Linos, E & Willett, W (2009) Meat, dairy, and breast cancer: do we have an answer? Am J Clin Nutr 90, 455–456.CrossRefGoogle ScholarPubMed
66. Wu, K , Sinha, R , Holmes, MD et al. (2010) Meat mutagens and breast cancer in postmenopausal women – a cohort analysis. Cancer Epidemiol Biomarkers Prev 19, 1301–1310.CrossRefGoogle ScholarPubMed
67. Kabat, GC , Cross, AJ , Park, Y et al. (2009) Meat intake and meat preparation in relation to risk of postmenopausal breast cancer in the NIH–AARP diet and health study. Int J Cancer 124, 2430–2435.CrossRefGoogle ScholarPubMed
68. Missmer, SA , Smith-Warner, SA , Spiegelman, D et al. (2002) Meat and dairy food consumption and breast cancer: a pooled analysis of cohort studies. Int J Epidemiol 31, 78–85.CrossRefGoogle ScholarPubMed
69. Pala, V , Krogh, V , Berrino, F et al. (2009) Meat, eggs, dairy products, and risk of breast cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Am J Clin Nutr 90, 602–612.CrossRefGoogle ScholarPubMed
70. Lee, JE , Spiegelman, D , Hunter, DJ et al. (2008) Fat, protein, and meat consumption and renal cell cancer risk: a pooled analysis of 13 prospective studies. J Natl Cancer Inst 100, 1695–1706.CrossRefGoogle ScholarPubMed
71. Larsson, SC , Hakanson, N , Permert, J et al. (2006) Meat, fish, poultry and egg consumption in relation to risk of pancreatic cancer: a prospective study. Int J Cancer 118, 2866–2870.CrossRefGoogle ScholarPubMed
72. Tasevska, N , Cross, AJ , Dodd, KW et al. (2010) No effect of meat, meat cooking preferences, meat mutagens or heme iron on lung cancer risk in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Int J Cancer.Google ScholarPubMed
73. Sinha, R , Park, Y , Graubard, BI et al. (2009) Meat and meat-related compounds and risk of prostate cancer in a large prospective cohort study in the United States. Am J Epidemiol 170, 1165–1177.CrossRefGoogle Scholar
74. Sinha, R , Cross, AJ , Graubard, BI et al. (2009) Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med 169, 562–571.CrossRefGoogle ScholarPubMed
75. Spencer, EA , Key, TJ , Appleby, PN et al. (2010) Meat, poultry and fish and risk of colorectal cancer: pooled analysis of data from the UK dietary cohort consortium. Cancer Causes Control (Epublication ahead of print version).CrossRefGoogle ScholarPubMed
78. Kantor, LS (1999) A comparison of the US food supply with the food guide pyramid recommendations. In American's Eating Habits: Changes and Consequences. Information Bulletin no. 750, pp. 71–95 [E Frazao, editor]. Washington, DC: USDA.Google Scholar
79. Sekula, W , Nelson, M , Figurska, K et al. (2005) Comparison between household budget survey and 24-hour recall data in a nationally representative sample of Polish households. Public Health Nutr 8, 430–439.CrossRefGoogle Scholar
80. Basiotis, PP , Welsh, SO , Cronin, FJ et al. (1987) Number of days of food intake records required to estimate individual and group nutrient intakes with defined confidence. J Nutr 117, 1638–1641.CrossRefGoogle ScholarPubMed
Source: https://www.cambridge.org/core/journals/public-health-nutrition/article/trends-in-meat-consumption-in-the-usa/AF54FD0E4A321394C09BC8087640AA0C
0 Response to "Udsa Beef Consumption by Year 1987"
Post a Comment